Low back pain is one of the most common reasons people visit a Physiotherapist. It can happen to anyone, at any age, and it often shows up without warning. However, the good news is that there are ways to relieve your pain and minimize the chances of it coming back. In this blog, we will explore what causes this type of pain, how to treat it, and how to keep it from becoming a regular problem.
What causes low back pain?
There are many reasons why you might have pain in your lower back. For example, some of the most common causes include:
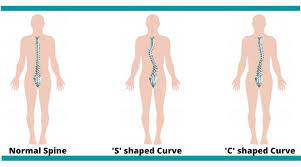
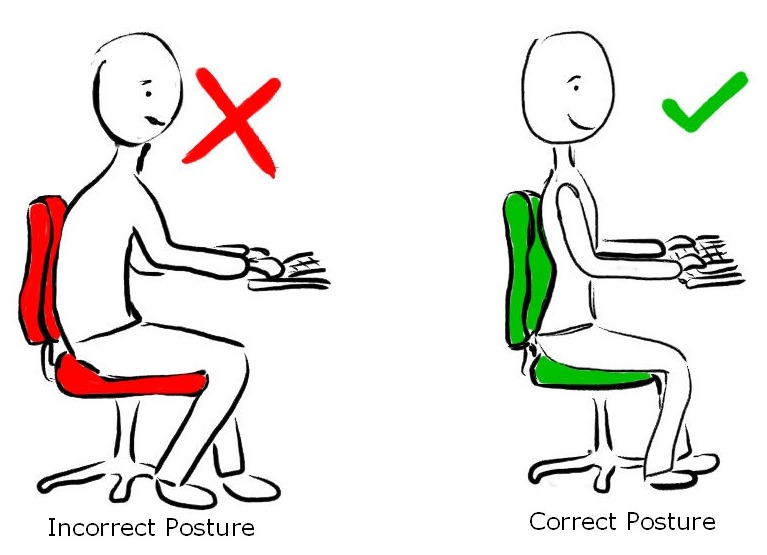
- Poor Posture: Sitting or standing with poor posture can put a lot of strain on the muscles and joints in your back. Consequently, over time, this can lead to pain and discomfort.
- Muscle Strain: Lifting something heavy, twisting awkwardly, or overdoing it during exercise can strain the muscles in your lower back. This can cause pain that may last for a few days or weeks.
- Inactivity: If you spend too much time sitting or lying down, your back muscles can become weaker. Weak muscles are more likely to get tired and painful, especially when you try to do something active again.
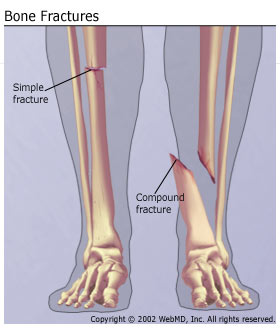
- Injuries: Falls, accidents, or sudden movements can injure the structures in your back, including the muscles, ligaments, and discs. Furthermore, these types of injuries can lead to long-lasting pain if not treated properly.
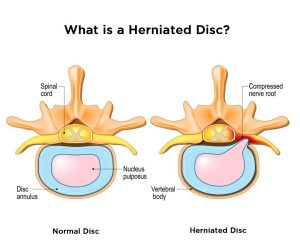
- Age-Related Changes: As we get older, our spine changes. Namely, the discs between our vertebrae can wear down, and arthritis can develop. This is called degenerative disc disease or osteoarthritis, and it can lead to low back pain.
Tips for Preventing Low Back Pain
Here are some simple steps you can take to minimize the risk and chances of having low back pain:
- Stay active: Regular physical activity keeps your muscles strong and flexible. For example, walking, swimming, and yoga are all great low impact ways to keep your back healthy.
- Lift safely: When lifting heavy objects, bend your knees and keep the object close to your body. Additionally, avoid twisting while lifting, as this puts further strain on your back in an already vulnerable position.
- Take breaks from sitting: If you work at a desk or sit for long periods of time, make sure to stand up and stretch every 30 minutes. Importantly, this helps reduce the pressure on your lower back. Alternatively, you may choose to have a standing desk so that you can switch between both positions.
- Sleep in a comfortable position: Sleeping on your side with a pillow between your knees can help keep your spine in a comfortable position. Additionally, make sure your mattress provides enough support for your back.
- Maintain a healthy weight: Extra weight, especially around your belly, can put more stress on your lower back. As a result, eating a balanced diet and staying active can help you maintain a healthy weight.
How can physiotherapy help?

Despite your best efforts to prevent it, if you are struggling with Low Back Pain, Physiotherapy is one of the most effective ways to manage a stubborn pain. A physiotherapist can help in the following ways:
- Pain relief techniques: Physiotherapists use various methods to help relieve pain, such as heat or ice
therapy, massage and manual therapy techniques, or electrical stimulation. These treatments can help reduce your pain and make you feel more comfortable. - Exercises to strengthen your back: Specific exercises can help strengthen the muscles in your back,
core, and legs. Strong muscles support your spine better and reduce the risk of future pain. Your
physiotherapist will show you exercises that are safe and effective for you. - Stretching: Next, tight muscles can contribute to back pain. Your physiotherapist will guide you through stretches that help improve flexibility in your back, hips, and legs, which can ease the pain and improve your overall movement.
- Posture correction: Importantly, learning how to stand, sit, and move correctly can make a big difference. A physiotherapist can teach you how to maintain good posture and reduce the strain on your back during everyday activities.
- Education: Sometimes, understanding what is causing your injury or condition can help reduce your worries about it. Accordingly, your physiotherapist will explain what’s happening in your back, what that means for you, and how you can manage the pain.
When should you see a physiotherapist for low back pain?
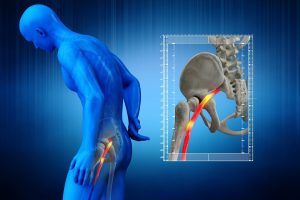
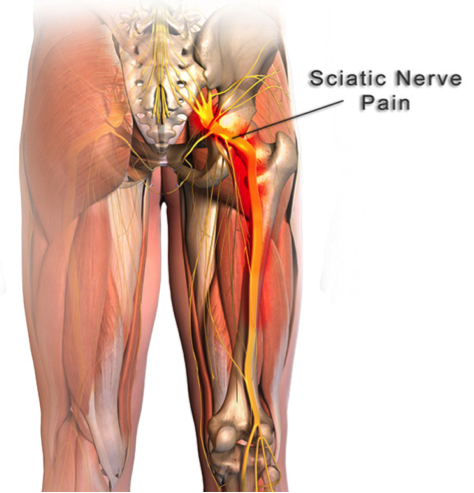
If your lower back doesn’t get better within a couple days to weeks, or if it continues to worsen, it’s a good idea to see a physiotherapist. Also, you should also seek help if you have other symptoms, such as pain going down your leg, numbness, or weakness. Fortunately, a physiotherapist can assess your condition and create a treatment plan that’s right for you. With the right treatment, education, and some simple lifestyle changes, you can manage the pain and get back to doing the things you love. If you’re struggling with low back pain, look for PhysioNow! Book with us today for your first assessment and treatment!